This article delves into the latest advancements in the treatment of neurological diseases, offering insights into innovative therapies, research breakthroughs, and expert opinions to enhance understanding and awareness.
Understanding Neurological Diseases
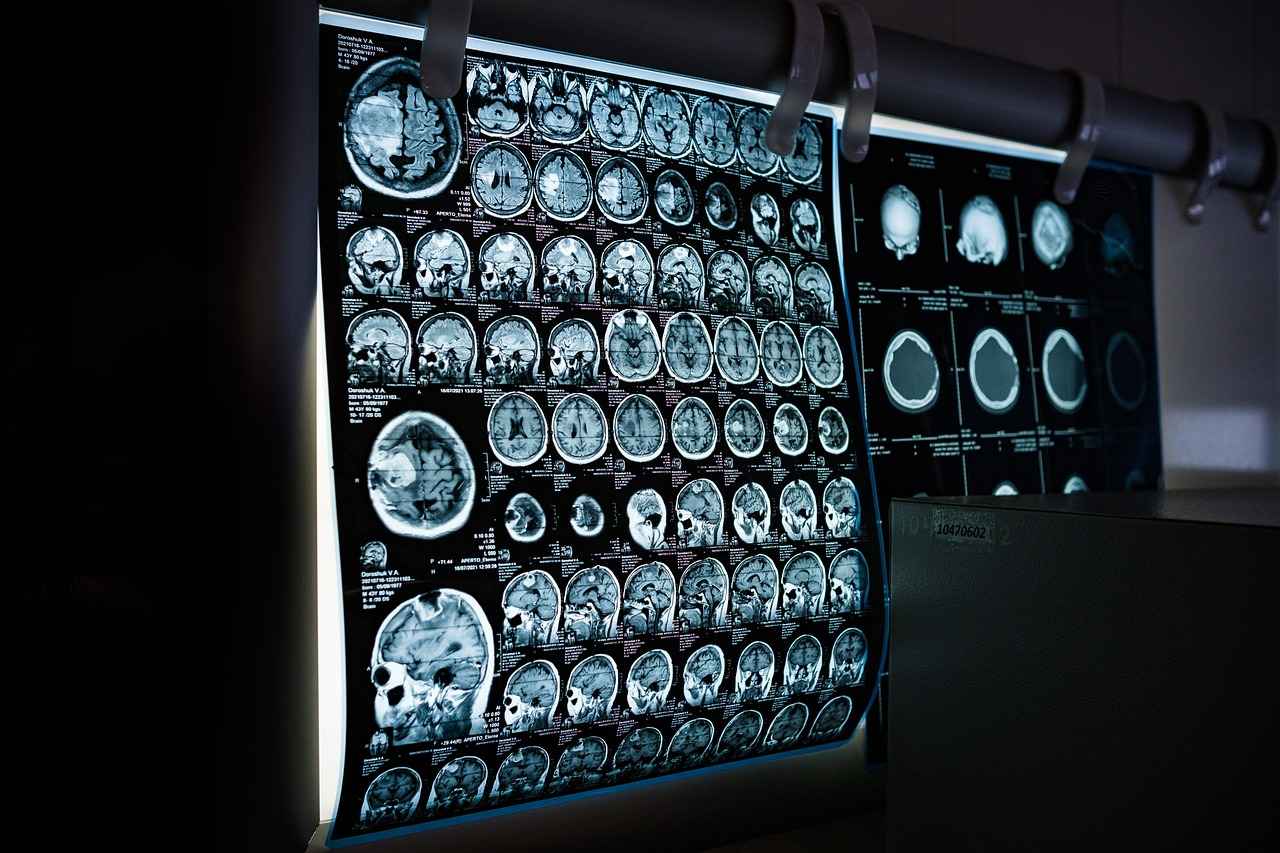
Neurological diseases encompass a wide range of disorders that affect the nervous system, including the brain, spinal cord, and peripheral nerves. These conditions can lead to significant physical and cognitive impairments, impacting individuals’ quality of life. Common symptoms include memory loss, movement disorders, and changes in behavior. Early diagnosis and intervention are crucial, as they can significantly improve outcomes and enhance the effectiveness of treatments.
Common Types of Neurological Disorders
- Alzheimer’s Disease: A progressive condition that leads to memory loss and cognitive decline.
- Parkinson’s Disease: Affects movement and coordination, characterized by tremors and stiffness.
- Multiple Sclerosis: An autoimmune disease that disrupts communication between the brain and the body.
Innovative Treatments for Neurological Disorders
Emerging treatments in neurology are reshaping patient care. Innovative approaches such as gene therapy, stem cell therapy, and neurostimulation techniques are being explored to address the underlying causes of neurological diseases. These therapies aim not only to alleviate symptoms but also to promote healing and recovery at a cellular level.
Gene Therapy in Neurology
Gene therapy represents a breakthrough in treating genetic neurological disorders. Technologies like CRISPR are utilized to correct genetic defects, offering potential cures for conditions previously deemed untreatable. Ongoing research is focused on translating these advancements into clinical practice, paving the way for personalized medicine in neurology.
Stem Cell Therapy Advancements
Stem cell therapy holds promise for neurodegenerative diseases by potentially regenerating damaged tissues. Current research and clinical trials are exploring the efficacy of stem cells in repairing neural pathways, which could revolutionize treatment options for conditions like Alzheimer’s and Parkinson’s. Ethical considerations surrounding stem cell use are also being addressed to ensure responsible application in medicine.
The Role of Lifestyle in Neurological Health
Lifestyle choices significantly impact neurological health. A balanced diet rich in essential nutrients, regular exercise, and mental health practices contribute to the prevention and management of neurological diseases. Holistic approaches to care are increasingly recognized for their effectiveness in supporting brain health.
Nutrition and Neurological Health
A balanced diet plays a crucial role in maintaining brain health. Nutrients such as omega-3 fatty acids, antioxidants, and vitamins E and D are essential for cognitive function. Dietary patterns like the Mediterranean diet have been linked to reduced risk of neurological disorders, emphasizing the importance of nutrition in brain health.
Exercise and Brain Function
Regular physical activity is associated with improved brain health. Exercise enhances cognitive function, reduces stress levels, and promotes overall neurological well-being. Engaging in activities like aerobic exercise, strength training, and even yoga can significantly benefit brain health and reduce the risk of developing neurological diseases.
Future Trends in Neurological Research
The landscape of neurological research is rapidly evolving, with cutting-edge studies focusing on innovative treatments and technologies. Artificial intelligence (AI) is transforming how neurological diseases are diagnosed and treated, enabling personalized treatment plans based on patient data analysis.
Artificial Intelligence in Neurology
AI is playing a crucial role in analyzing patient data and predicting disease progression. Machine learning algorithms can identify patterns that may not be visible to human clinicians, facilitating early diagnosis and tailored treatment strategies. This technology holds great promise for enhancing patient outcomes in neurology.
Telemedicine in Neurological Care
Telemedicine has become increasingly important in neurology, especially in the wake of the COVID-19 pandemic. Virtual consultations improve access to care, allowing patients to receive ongoing management of their neurological conditions from the comfort of their homes. This shift has the potential to enhance patient engagement and adherence to treatment plans.

Understanding Neurological Diseases
Neurological diseases are a complex group of disorders that significantly affect the nervous system, which includes the brain, spinal cord, and peripheral nerves. These conditions can lead to a variety of symptoms and complications, impacting an individual’s overall health and quality of life. Understanding these diseases is crucial for timely diagnosis and effective management.
Classification of Neurological Diseases
Neurological diseases can be broadly classified into several categories:
- Degenerative Disorders: Conditions such as Alzheimer’s disease and Parkinson’s disease that progressively worsen over time.
- Vascular Disorders: These include stroke and transient ischemic attacks (TIAs), which are caused by blood flow issues to the brain.
- Infectious Diseases: Conditions like meningitis and encephalitis that result from infections affecting the nervous system.
- Autoimmune Disorders: Diseases such as multiple sclerosis, where the immune system mistakenly attacks healthy nerve tissues.
- Congenital Disorders: Neurological issues present at birth, such as spina bifida and cerebral palsy.
Common Symptoms of Neurological Diseases
The symptoms of neurological diseases can vary widely depending on the specific disorder and the areas of the nervous system affected. Common symptoms include:
- Cognitive Impairment: Memory loss, confusion, and difficulty concentrating.
- Motor Dysfunction: Weakness, tremors, and coordination problems.
- Sensory Changes: Numbness, tingling, or pain in various body parts.
- Emotional Disturbances: Depression, anxiety, and mood swings.
Impact on Individuals’ Lives
The effects of neurological diseases extend beyond physical symptoms, often leading to significant emotional and social challenges. Individuals may experience:
- Loss of Independence: Many neurological conditions impair daily functioning, necessitating assistance with routine tasks.
- Social Isolation: Symptoms may limit social interactions, leading to feelings of loneliness and despair.
- Financial Burden: Ongoing medical care, therapy, and possible loss of employment can create financial strain on individuals and families.
Importance of Early Diagnosis and Treatment
Early diagnosis of neurological diseases is crucial for effective management and improved outcomes. Timely intervention can:
- Slow Disease Progression: Early treatment may slow the advancement of conditions like Alzheimer’s and Parkinson’s.
- Enhance Quality of Life: Managing symptoms effectively can lead to better daily functioning and overall well-being.
- Facilitate Support Systems: Early diagnosis allows for the establishment of support networks, including healthcare providers and community resources.
In conclusion, understanding neurological diseases is vital for recognizing symptoms, seeking appropriate medical care, and improving the quality of life for those affected. Ongoing research and advancements in treatment options continue to offer hope for better management of these complex disorders.

Common Types of Neurological Disorders
This section delves into the , focusing on conditions that significantly impact millions of lives worldwide. Understanding these disorders is essential for early detection, effective management, and improved patient outcomes. Below, we explore three of the most prevalent neurological disorders: Alzheimer’s disease, Parkinson’s disease, and multiple sclerosis.
Alzheimer’s disease is a progressive neurodegenerative disorder primarily characterized by memory loss, cognitive decline, and behavioral changes. It predominantly affects older adults, with symptoms often beginning subtly and gradually worsening over time. Early signs may include forgetfulness, confusion about time and place, and difficulty completing familiar tasks.
As the disease progresses, individuals may experience severe memory impairment, challenges in communication, and changes in personality. Understanding these symptoms is crucial for timely diagnosis and intervention. Current research focuses on identifying biomarkers for early detection and developing treatments that target the underlying mechanisms of the disease.
Parkinson’s disease is another prevalent neurological disorder that affects movement and coordination. It is characterized by tremors, stiffness, slowness of movement, and balance difficulties. The exact cause remains unclear, but it is believed to involve a combination of genetic and environmental factors.
Patients often experience a gradual progression of symptoms, which can significantly affect daily activities. Early recognition of symptoms is vital for initiating treatment strategies, which may include medications, physical therapy, and, in some cases, surgical interventions such as deep brain stimulation. Ongoing research aims to find neuroprotective therapies that can slow disease progression.
Multiple sclerosis (MS) is an autoimmune disorder that affects the central nervous system. It occurs when the immune system mistakenly attacks the protective covering of nerve fibers, leading to communication problems between the brain and the rest of the body. Symptoms can vary widely, including fatigue, difficulty walking, numbness, and vision problems.
MS is characterized by periods of relapses and remissions, making it essential for individuals to recognize their symptoms and seek appropriate care. Current treatment options focus on managing symptoms and modifying the disease course through disease-modifying therapies (DMTs). Research is ongoing to explore new therapies and improve patient quality of life.
Understanding these neurological disorders is vital for recognizing symptoms and seeking timely medical intervention. Early diagnosis can significantly impact treatment effectiveness and overall quality of life. Individuals experiencing symptoms related to these conditions should consult healthcare professionals for comprehensive evaluations and personalized treatment plans.
In conclusion, awareness of common neurological disorders such as Alzheimer’s, Parkinson’s, and multiple sclerosis is crucial for effective management and support. By understanding the symptoms and available treatments, patients and caregivers can take proactive steps towards better neurological health.
Alzheimer’s Disease
is a complex condition that affects millions of people worldwide. As a progressive neurodegenerative disorder, it primarily impacts memory, thinking, and behavior. Understanding the various stages of Alzheimer’s, its symptoms, and the latest research on potential treatments is crucial for patients, caregivers, and healthcare professionals alike. This section aims to provide a comprehensive overview of these aspects, shedding light on the current landscape of Alzheimer’s disease management.
Alzheimer’s disease progresses through several distinct stages, each characterized by specific symptoms and challenges:
- Early Stage: In the initial phase, individuals may experience mild memory loss and difficulty in concentrating. They might forget recent conversations or misplace items.
- Moderate Stage: As the disease progresses, symptoms become more pronounced. Individuals may struggle with familiar tasks, experience confusion about time and place, and exhibit changes in personality.
- Severe Stage: In the final stages, individuals may lose the ability to communicate and require assistance with daily activities. Memory loss becomes profound, and physical abilities may decline significantly.
Recognizing the symptoms of Alzheimer’s is vital for early diagnosis. Common symptoms include:
- Memory Loss: Difficulty remembering recent events or important dates.
- Difficulty with Problem-Solving: Struggles with planning or solving everyday problems.
- Confusion: Getting lost in familiar places or having trouble understanding visual images.
- Personality Changes: Mood swings, withdrawal from social activities, and increased anxiety.
Recent advancements in Alzheimer’s research have led to promising developments in treatment options. Researchers are exploring various avenues, including:
- Medications: Currently, FDA-approved medications like donepezil and memantine help manage symptoms but do not halt disease progression. Ongoing studies are investigating new drugs that may target the underlying causes of Alzheimer’s.
- Immunotherapy: This innovative approach aims to harness the body’s immune system to combat Alzheimer’s pathology, particularly targeting amyloid-beta plaques that disrupt neuronal function.
- Gene Therapy: Researchers are investigating gene editing technologies, such as CRISPR, to correct genetic mutations associated with familial Alzheimer’s disease, offering potential for more effective treatments.
While genetics play a significant role in Alzheimer’s, lifestyle choices can also impact the risk of developing the disease. Key lifestyle changes include:
- Healthy Diet: Diets rich in antioxidants, omega-3 fatty acids, and low in processed sugars can support brain health.
- Regular Exercise: Physical activity has been linked to improved cognitive function and may reduce the risk of dementia.
- Mental Stimulation: Engaging in puzzles, reading, and learning new skills can help maintain cognitive function.
In conclusion, understanding Alzheimer’s disease is essential for effective management and care. Ongoing research continues to unveil new treatment possibilities, while lifestyle modifications can play a crucial role in prevention and overall brain health. By staying informed and proactive, individuals can better navigate the challenges posed by this complex disorder.
Current Treatments for Alzheimer’s
Alzheimer’s disease, a complex and multifaceted neurodegenerative disorder, presents significant challenges not only for patients but also for their families and caregivers. The current treatment landscape primarily focuses on managing symptoms and enhancing the quality of life for those affected. This section will delve into the FDA-approved medications available today, as well as emerging therapies that aim to address the underlying pathology of the disease.
Currently, there are several FDA-approved medications that fall into two main categories: cholinesterase inhibitors and NMDA receptor antagonists. Cholinesterase inhibitors, such as Donepezil, Rivastigmine, and Galantamine, work by increasing levels of acetylcholine, a neurotransmitter associated with memory and learning. These medications can help alleviate symptoms related to memory loss and cognitive decline, particularly in the early to moderate stages of the disease.
- Donepezil: Commonly prescribed for all stages of Alzheimer’s, it has been shown to improve cognitive function and slow the progression of symptoms.
- Rivastigmine: Available as a patch or oral medication, it is particularly effective for patients with mild to moderate Alzheimer’s.
- Galantamine: This medication not only increases acetylcholine levels but also modulates nicotinic receptors, which may enhance cognitive processing.
The second category, NMDA receptor antagonists, includes Memantine. This medication works differently by regulating glutamate activity, which is crucial for learning and memory. Memantine is often prescribed for moderate to severe Alzheimer’s and can be used in conjunction with cholinesterase inhibitors to provide a more comprehensive approach to symptom management.
In addition to these established treatments, ongoing research is paving the way for innovative therapies that target the underlying mechanisms of Alzheimer’s disease. One promising avenue is immunotherapy, which aims to harness the body’s immune system to combat the amyloid plaques and tau tangles characteristic of Alzheimer’s pathology. Clinical trials are exploring various immunotherapeutic agents, such as monoclonal antibodies, which have shown potential in reducing amyloid burden in the brain.
Another exciting area of research involves gene therapy. Scientists are investigating the potential of gene editing technologies, such as CRISPR, to correct genetic mutations that may contribute to Alzheimer’s disease. While still in the experimental stages, these approaches hold promise for future treatments that could alter the course of the disease.
As we look to the future, it is essential to remain optimistic about the advancements in Alzheimer’s research. With a growing understanding of the disease’s underlying mechanisms, the development of targeted therapies may soon lead to more effective treatments that not only manage symptoms but also address the root causes of Alzheimer’s disease.
Future Directions in Alzheimer’s Research
Research into Alzheimer’s disease is experiencing a transformative phase, with scientists and medical professionals exploring various innovative strategies that hold the potential to revolutionize treatment options. As we delve into the , two particularly promising avenues are immunotherapy and gene therapy.
Immunotherapy has emerged as a beacon of hope in recent years. This approach harnesses the body’s immune system to target and eliminate the toxic proteins associated with Alzheimer’s, such as amyloid-beta and tau. By utilizing monoclonal antibodies, researchers aim to enhance the immune response against these proteins. Clinical trials have shown that immunotherapy can reduce amyloid plaques in the brain, potentially slowing cognitive decline. Notable candidates include drugs like aducanumab, which has sparked significant interest and debate within the medical community. As research progresses, optimizing the timing and dosage of these therapies could unlock their full potential, leading to more effective treatment protocols.
Meanwhile, gene therapy represents another groundbreaking frontier in Alzheimer’s research. This technique involves modifying or replacing defective genes responsible for the disease’s progression. With advancements in gene editing technologies, particularly CRISPR-Cas9, scientists are exploring ways to correct genetic mutations that predispose individuals to Alzheimer’s. For instance, researchers are investigating the possibility of delivering genes that encode for protective proteins directly into the brain, thereby enhancing neuronal survival and function. Early-stage trials have indicated that such interventions could lead to significant improvements in cognitive function and overall brain health.
Additionally, the integration of biomarkers into Alzheimer’s research is gaining traction. Biomarkers can provide critical insights into disease progression and treatment efficacy. By identifying specific biological indicators, researchers can stratify patients based on their unique disease profiles, enabling more personalized and targeted therapies. This approach not only enhances the precision of clinical trials but also paves the way for earlier interventions, which are crucial in managing Alzheimer’s effectively.
Moreover, the role of neuroinflammation in Alzheimer’s is being increasingly recognized. Understanding how inflammation contributes to neuronal damage opens new therapeutic avenues. Researchers are investigating anti-inflammatory agents that could mitigate the neuroinflammatory response, potentially slowing disease progression and improving patient outcomes.
As we look ahead, collaboration between researchers, clinicians, and industry stakeholders will be vital in translating these promising findings into clinical practice. The convergence of technological advancements, such as artificial intelligence and machine learning, is also expected to enhance our understanding of Alzheimer’s disease and streamline drug discovery processes.
In conclusion, the future of Alzheimer’s research is bright, with immunotherapy and gene therapy leading the charge. As ongoing studies continue to unfold, the hope for more effective treatments grows stronger, offering renewed optimism for patients and families affected by this devastating disease.
Parkinson’s Disease
is a progressive neurological disorder that primarily affects movement and coordination. It occurs when the nerve cells in the brain that produce dopamine, a neurotransmitter responsible for sending messages to the part of the brain that controls movement, gradually deteriorate. This section delves into the symptoms, progression, and the latest therapeutic approaches available for managing Parkinson’s disease, including medication adjustments and innovative surgical interventions like deep brain stimulation.
Symptoms of Parkinson’s Disease
- Tremors: Often the first noticeable symptom, tremors can occur when the muscles are at rest.
- Bradykinesia: This refers to slowness of movement, making everyday tasks more challenging.
- Muscle Stiffness: Stiffness in the limbs and trunk can limit flexibility and range of motion.
- Postural Instability: Balance issues may develop, leading to an increased risk of falls.
- Non-Motor Symptoms: These can include sleep disturbances, depression, and cognitive changes.
Progression of Parkinson’s Disease
The progression of Parkinson’s disease varies significantly among individuals. It is typically categorized into five stages:
- Stage 1: Mild symptoms that do not interfere with daily activities.
- Stage 2: Symptoms worsen, affecting both sides of the body, with noticeable difficulties in daily tasks.
- Stage 3: Significant impairment in balance and coordination; individuals may experience falls.
- Stage 4: Severe symptoms, requiring assistance with daily activities.
- Stage 5: The most advanced stage, often resulting in complete dependence on caregivers.
Therapeutic Approaches
Management of Parkinson’s disease often involves a combination of medication and surgical options. Medications such as Levodopa are commonly prescribed to replenish dopamine levels, while other drugs may help manage symptoms. Adjustments in medication can be critical as the disease progresses, necessitating ongoing communication between patients and healthcare providers.
Surgical Interventions
For some patients, deep brain stimulation (DBS) may be a viable option. This surgical procedure involves implanting electrodes in specific brain regions, which are then stimulated to alleviate symptoms. DBS has shown promising results in reducing tremors and improving overall quality of life for many patients.
In summary, understanding Parkinson’s disease is essential for effective management and treatment. With ongoing research and advancements in therapeutic approaches, individuals living with this condition can find hope and support in their journey.

Innovative Treatments for Neurological Disorders
In recent years, the field of neurology has witnessed a surge of innovative treatments that are fundamentally changing how neurological disorders are managed. These advancements not only aim to alleviate symptoms but also target the underlying causes of diseases, leading to more effective and lasting solutions for patients. This section delves into three groundbreaking approaches: gene therapy, stem cell therapy, and neurostimulation techniques.
Gene Therapy: A New Frontier in Neurology
Gene therapy is revolutionizing the treatment landscape for genetic neurological disorders. By utilizing advanced technologies such as CRISPR and viral vectors, researchers are developing methods to correct genetic defects at their source. This approach holds promise for conditions like Huntington’s disease and certain forms of muscular dystrophy. Clinical trials have shown that delivering healthy copies of genes directly to affected areas can lead to significant improvements in patient outcomes.
Moreover, gene therapy is not limited to hereditary conditions. It is also being explored for acquired neurological disorders, such as multiple sclerosis, where the immune system attacks the nervous system. By modulating immune responses through targeted gene delivery, researchers hope to slow disease progression and improve quality of life for patients.
Stem Cell Therapy: Regenerating Damaged Tissues
Stem cell therapy represents a beacon of hope for those suffering from neurodegenerative diseases like Alzheimer’s and Parkinson’s. The ability of stem cells to differentiate into various cell types makes them ideal candidates for repairing damaged neural tissues. Current research is focusing on the use of both embryonic and adult stem cells to regenerate neurons and restore lost functions.
Clinical trials are underway to assess the safety and efficacy of stem cell treatments. Preliminary results have shown promising outcomes, with some patients experiencing improved motor functions and cognitive abilities. However, ethical considerations and the need for rigorous regulatory frameworks remain paramount as this field evolves.
Neurostimulation Techniques: A Non-Invasive Approach
Neurostimulation techniques, including transcranial magnetic stimulation (TMS) and deep brain stimulation (DBS), are gaining traction as effective treatments for various neurological disorders. TMS is a non-invasive method that uses magnetic fields to stimulate nerve cells in the brain, showing efficacy in treating depression and chronic pain.
On the other hand, DBS involves implanting electrodes in specific brain regions to modulate abnormal activity. This technique has been particularly successful in treating Parkinson’s disease, providing significant relief from tremors and rigidity. As technology advances, the future of neurostimulation holds the potential for even more precise and personalized therapies.
In conclusion, the landscape of neurological treatment is evolving rapidly, with innovative therapies paving the way for improved patient care. As research continues to advance, these novel approaches promise to enhance the quality of life for individuals affected by neurological disorders.
Gene Therapy in Neurology
Gene therapy has emerged as a revolutionary approach in the treatment of various genetic neurological disorders. This innovative technique focuses on altering the genes within an individual’s cells to treat or prevent disease. By utilizing advanced technologies such as CRISPR (Clustered Regularly Interspaced Short Palindromic Repeats), researchers are now able to precisely target and modify faulty genes, offering hope for conditions that were once deemed untreatable.
The potential of gene therapy lies in its ability to address the root causes of genetic disorders. For instance, conditions like Huntington’s disease and certain forms of muscular dystrophy are caused by specific genetic mutations. By employing gene editing technologies, scientists can potentially correct these mutations, restoring normal function to the affected genes. This approach not only aims to alleviate symptoms but also targets the underlying genetic issues, potentially leading to a cure.
One of the most significant advancements in gene therapy is the use of CRISPR technology. CRISPR allows for precise editing of the genome, enabling researchers to remove, add, or alter sections of DNA. This has opened up new avenues for treating neurological disorders. For example, studies are underway to use CRISPR to modify genes responsible for neurodegenerative diseases, which could halt or even reverse disease progression.
Clinical trials are currently exploring the effectiveness and safety of gene therapy in various neurological conditions. In one promising study, researchers are investigating the use of gene therapy to deliver healthy copies of genes directly to brain cells affected by Alzheimer’s disease. Early results indicate that this approach may improve cognitive function and slow disease progression.
However, the journey of gene therapy is not without challenges. Ethical considerations, potential side effects, and the need for long-term studies to assess the efficacy and safety of these treatments are critical aspects that researchers must address. As we move forward, collaboration between scientists, clinicians, and regulatory bodies will be essential to ensure that gene therapy can be safely integrated into clinical practice.
In conclusion, gene therapy represents a significant leap forward in the treatment of genetic neurological disorders. With ongoing research and clinical trials, the potential to correct genetic defects and offer cures for previously untreatable conditions is becoming increasingly tangible. As we continue to unlock the mysteries of our genetic code, the future of neurology may be transformed by these groundbreaking therapies.
Stem Cell Therapy Advancements
Stem cell therapy is emerging as a revolutionary approach in the treatment of neurodegenerative diseases, offering hope for patients with conditions such as Alzheimer’s and Parkinson’s. This innovative therapy aims to regenerate damaged neural tissues and restore lost functions by utilizing the unique properties of stem cells. In this section, we will delve into the latest research, ongoing clinical trials, and the ethical considerations surrounding the use of stem cells in neurology.
Current Research in Stem Cell Therapy
Recent studies have demonstrated the potential of stem cells to differentiate into various types of neural cells, which can replace damaged or lost neurons. Research is ongoing in several key areas:
- Induced Pluripotent Stem Cells (iPSCs): Scientists are exploring the use of iPSCs derived from adult cells, which can be transformed into any cell type, including neurons. This approach minimizes ethical concerns associated with embryonic stem cells.
- Mesenchymal Stem Cells (MSCs): MSCs, found in bone marrow and adipose tissue, are being investigated for their ability to modulate inflammation and promote healing in neurodegenerative conditions.
- Neural Stem Cells (NSCs): NSCs are being studied for their direct application in repairing damaged brain tissues, particularly in stroke and traumatic brain injury cases.
Clinical Trials and Their Impact
Numerous clinical trials are currently underway to assess the safety and efficacy of stem cell therapies for neurological disorders. For instance, trials involving the transplantation of stem cells into patients with Parkinson’s disease have shown promising results, with some participants experiencing significant improvements in motor function. Additionally, studies on Alzheimer’s patients receiving stem cell infusions are exploring the potential to halt or even reverse cognitive decline.
Ethical Considerations
Despite the promise of stem cell therapy, ethical concerns persist. The primary issues revolve around the source of stem cells, particularly when derived from embryos. However, advancements in iPSC technology have provided a viable alternative, alleviating some ethical dilemmas. It’s essential for researchers and clinicians to navigate these ethical waters carefully, ensuring that patient welfare remains a priority while advancing scientific knowledge.
Future Directions in Stem Cell Research
The future of stem cell therapy in neurology looks promising. Researchers are exploring combination therapies, where stem cell treatment is paired with other modalities like gene therapy or neuroprotective drugs. This integrative approach could enhance therapeutic outcomes and provide more comprehensive care for patients suffering from neurodegenerative diseases.
In conclusion, stem cell therapy represents a beacon of hope in the field of neurology, with ongoing research and clinical trials paving the way for innovative treatment options. As we continue to uncover the potential of stem cells, it is crucial to maintain ethical standards and prioritize patient safety in this evolving landscape.
The Role of Lifestyle in Neurological Health
Lifestyle choices play a crucial role in maintaining and enhancing neurological health. Research shows that factors such as diet, exercise, and mental well-being significantly influence the prevention and management of neurological diseases. By adopting a holistic approach to care, individuals can improve their cognitive function and overall brain health.
A well-balanced diet is essential for optimal brain function. Nutritional neuroscience has identified several key nutrients that support cognitive health:
- Omega-3 Fatty Acids: Found in fish, flaxseeds, and walnuts, these fatty acids are known to promote brain health and may reduce the risk of Alzheimer’s disease.
- Antioxidants: Foods rich in antioxidants, such as berries and dark chocolate, help combat oxidative stress, which is linked to neurodegenerative diseases.
- B Vitamins: Vitamins B6, B12, and folate are crucial for maintaining healthy brain function and may help in reducing the risk of cognitive decline.
Incorporating these nutrients into your diet can lead to improved memory, concentration, and overall cognitive abilities.
Regular physical activity is not only beneficial for physical health but also plays a vital role in enhancing brain function. Studies have shown that:
- Exercise Increases Blood Flow: Physical activity enhances blood circulation, ensuring that the brain receives sufficient oxygen and nutrients.
- Neurogenesis: Engaging in regular exercise promotes the growth of new neurons, particularly in the hippocampus, an area critical for learning and memory.
- Stress Reduction: Exercise helps reduce stress and anxiety, which are known to negatively impact cognitive function.
Incorporating at least 150 minutes of moderate exercise per week can significantly boost brain health and reduce the risk of neurological disorders.
Mental health is intricately connected to neurological health. Conditions such as depression and anxiety can exacerbate neurological issues and lead to cognitive decline. Strategies to maintain mental well-being include:
- Mindfulness and Meditation: These practices have been shown to improve focus, reduce stress, and enhance overall mental health.
- Social Connections: Maintaining strong social ties can provide emotional support and reduce feelings of isolation, which are detrimental to mental health.
- Cognitive Behavioral Therapy (CBT): This therapeutic approach can help individuals manage stress and anxiety, promoting better mental health outcomes.
By prioritizing mental health, individuals can create a positive feedback loop that enhances both psychological and neurological well-being.
In conclusion, the interplay between lifestyle choices and neurological health is profound. By focusing on a balanced diet, regular exercise, and mental well-being, individuals can take proactive steps to enhance their brain health and mitigate the risk of neurological diseases. Embracing a holistic approach to care not only fosters better cognitive function but also contributes to a higher quality of life.
Nutrition and Neurological Health
A balanced diet is essential for maintaining brain health and optimizing cognitive function. The brain, being one of the most energy-demanding organs in the body, requires a variety of nutrients to function effectively. This section will explore the critical nutrients that contribute to neurological health, dietary patterns that support cognitive function, and how these can potentially reduce the risk of neurological disorders.
One of the most important nutrients for brain health is omega-3 fatty acids. These healthy fats are primarily found in fish, flaxseeds, and walnuts. They are vital for building cell membranes in the brain and have been linked to improved memory and cognitive performance. Studies suggest that a diet rich in omega-3s may also lower the risk of developing Alzheimer’s disease and other forms of dementia.
Another key nutrient is antioxidants, which help combat oxidative stress in the brain. Foods rich in antioxidants include berries, dark chocolate, and leafy greens. Regular consumption of these foods can protect brain cells from damage and may even enhance neuroplasticity—the brain’s ability to reorganize itself by forming new neural connections throughout life.
B vitamins, particularly B6, B12, and folate, are also crucial for maintaining cognitive health. These vitamins play a role in producing neurotransmitters, which are essential for communication between brain cells. A deficiency in B vitamins has been linked to cognitive decline and increased risk of neurological disorders.
In addition to specific nutrients, certain dietary patterns can significantly impact brain health. The Mediterranean diet, which emphasizes whole grains, fruits, vegetables, fish, and healthy fats, has been associated with a reduced risk of cognitive decline. This diet is rich in nutrients that promote brain health and has been shown to improve memory and cognitive function.
Moreover, staying adequately hydrated is often overlooked but is essential for optimal brain function. Dehydration can lead to difficulties in concentration, memory, and overall cognitive performance. Therefore, it is vital to drink enough water throughout the day.
Incorporating a variety of these nutrient-rich foods into your daily diet can create a powerful defense against neurological disorders. Regular meals that include a mix of fruits, vegetables, whole grains, lean proteins, and healthy fats can provide the brain with the necessary fuel to function at its best.
Furthermore, it is essential to limit the intake of processed foods and sugars, as they can contribute to inflammation and oxidative stress, which are detrimental to brain health. Instead, focusing on whole foods that are minimally processed can promote better cognitive function and overall well-being.
In conclusion, a well-rounded diet rich in essential nutrients, antioxidants, and healthy fats is critical for maintaining neurological health. By prioritizing these dietary choices, individuals can support their brain function and potentially lower the risk of developing neurological disorders.
Exercise and Brain Function
Engaging in regular physical activity is not just beneficial for physical health; it plays a crucial role in enhancing brain function as well. Numerous studies have demonstrated that exercise can lead to significant improvements in cognitive abilities, emotional regulation, and overall neurological health. This section delves into the multifaceted ways in which exercise impacts the brain.
Enhancing Cognitive Function through Exercise
One of the most compelling benefits of exercise is its ability to enhance cognitive function. Physical activity increases blood flow to the brain, which can help to stimulate the growth of new neurons—a process known as neurogenesis. Activities such as aerobic exercises, strength training, and even yoga have been shown to improve memory, attention, and problem-solving skills. For instance, a study published in the journal Neuropsychology Review found that individuals who engaged in regular aerobic exercise performed better on cognitive tasks compared to those who were sedentary.
Reducing Stress and Anxiety
Exercise is also a powerful tool for reducing stress and anxiety levels. When we exercise, the body releases endorphins, often referred to as “feel-good” hormones. These endorphins can help alleviate feelings of depression and anxiety, contributing to a more stable emotional state. Furthermore, regular physical activity has been linked to lower levels of cortisol, the body’s primary stress hormone. Engaging in activities such as running, swimming, or even brisk walking can serve as an effective outlet for stress management.
Improving Overall Neurological Well-Being
In addition to enhancing cognitive abilities and reducing stress, exercise contributes to overall neurological well-being. Regular physical activity has been associated with a lower risk of developing neurodegenerative diseases such as Alzheimer’s and Parkinson’s. The mechanisms behind this protective effect include improved blood circulation, reduced inflammation, and enhanced brain plasticity. A meta-analysis published in the journal Ageing Research Reviews highlighted that individuals who maintain an active lifestyle have a significantly lower risk of cognitive decline as they age.
Types of Exercises Beneficial for Brain Health
- Aerobic Exercises: Activities like running, cycling, and swimming are particularly effective.
- Strength Training: Lifting weights or resistance training can also have cognitive benefits.
- Mind-Body Exercises: Practices such as yoga and tai chi promote mindfulness and stress reduction.
Conclusion
In summary, incorporating regular exercise into your routine can lead to significant improvements in brain health. From enhancing cognitive function and reducing stress to promoting overall neurological well-being, the benefits of physical activity are profound. As research continues to unveil the intricate connections between exercise and brain health, it becomes increasingly clear that staying active is essential for maintaining cognitive vitality throughout life.
Future Trends in Neurological Research
The field of neurology is witnessing unprecedented advancements, driven by innovative research and technological integration. As we explore the **future trends** in neurological research, it is essential to understand how these developments may transform treatment approaches, enhance diagnostic accuracy, and ultimately improve patient outcomes.
Artificial Intelligence: Revolutionizing Neurology
Artificial intelligence (AI) is becoming a cornerstone in the diagnosis and treatment of neurological disorders. Machine learning algorithms are being developed to analyze vast amounts of patient data, enabling clinicians to identify patterns that may not be visible to the human eye. For instance, AI can assist in early detection of conditions like Alzheimer’s disease by analyzing changes in brain scans over time. This capability not only facilitates earlier interventions but also allows for more personalized treatment plans tailored to individual patient needs.
Telemedicine: Expanding Access to Care
The rise of telemedicine has been accelerated by the COVID-19 pandemic, and its impact on neurological care is significant. Virtual consultations are breaking down geographical barriers, allowing patients to access specialists without the need for travel. This trend is particularly beneficial for individuals living in rural areas or those with mobility challenges. Furthermore, telemedicine platforms are integrating remote monitoring tools that enable continuous assessment of neurological conditions, ensuring timely adjustments to treatment regimens.
Neurogenomics: Understanding the Genetic Basis of Neurological Disorders
Neurogenomics is an emerging field that examines the relationship between genetics and neurological diseases. With advancements in genomic sequencing technologies, researchers are uncovering genetic mutations linked to conditions such as Parkinson’s and Huntington’s disease. This knowledge is paving the way for targeted therapies that address the underlying genetic causes of these disorders. As we gain a deeper understanding of the genetic factors involved, the potential for personalized medicine in neurology becomes increasingly viable.
Regenerative Medicine: The Promise of Stem Cells
Regenerative medicine, particularly stem cell therapy, is at the forefront of neurological research. Scientists are investigating how stem cells can repair or regenerate damaged neural tissues, offering hope for conditions like multiple sclerosis and spinal cord injuries. Clinical trials are underway to assess the efficacy and safety of these treatments, with preliminary results showing promise in restoring functionality and improving quality of life for patients.
Neurotechnology: Enhancing Brain Function
The integration of neurotechnology into clinical practice is another exciting trend. Devices such as brain-computer interfaces (BCIs) are being developed to assist individuals with severe mobility impairments. These technologies allow users to control devices through thought alone, significantly enhancing their independence and quality of life. Additionally, neurostimulation techniques are being researched for their potential to alleviate symptoms of various neurological disorders, including chronic pain and epilepsy.
Big Data and Neurology: A New Era of Research
The advent of big data analytics is transforming neurological research. By aggregating data from diverse sources, including electronic health records, genetic databases, and wearable health devices, researchers can identify trends and correlations that were previously unattainable. This comprehensive approach enables the discovery of new biomarkers for diseases, enhancing diagnostic capabilities and informing treatment strategies.
Ethical Considerations in Neurological Research
As we embrace these advancements, it is crucial to address the ethical implications surrounding neurological research. Issues such as data privacy, informed consent, and the equitable distribution of emerging therapies must be carefully considered. Engaging stakeholders, including patients, healthcare professionals, and ethicists, is essential to navigate these challenges and ensure that advancements in neurology benefit all individuals.
In summary, the future of neurological research is bright, with numerous trends poised to reshape the landscape of treatment and care. As we harness the power of technology and deepen our understanding of the brain, we move closer to a future where neurological disorders are managed more effectively, ultimately improving the lives of millions. The integration of AI, telemedicine, neurogenomics, regenerative medicine, and neurotechnology represents a holistic approach to addressing the complexities of neurological diseases, ensuring that we remain at the forefront of innovation in this critical field.
Artificial Intelligence in Neurology
Artificial Intelligence (AI) is revolutionizing the field of neurology by enhancing the way neurological diseases are diagnosed and treated. The integration of AI technologies, particularly machine learning, is enabling healthcare professionals to analyze vast amounts of patient data efficiently. This advancement is crucial as it allows for more accurate predictions of disease progression and facilitates the development of personalized treatment plans tailored to individual patient needs.
One of the most significant contributions of AI in neurology is its ability to process and analyze complex datasets, which include medical histories, genetic information, and imaging results. By employing sophisticated algorithms, AI can identify patterns and correlations that may not be immediately apparent to human clinicians. This capability is particularly beneficial in diagnosing conditions such as Alzheimer’s disease and Parkinson’s disease, where early detection is vital for effective management.
Moreover, machine learning models can predict disease trajectories, allowing neurologists to anticipate changes in a patient’s condition. For instance, AI can analyze data from wearable devices that monitor motor functions and cognitive performance, providing real-time insights into a patient’s health status. This predictive capability enables healthcare providers to adjust treatment strategies proactively, ensuring that interventions are timely and appropriate.
AI is also playing a pivotal role in clinical trials for new neurological treatments. By using predictive analytics, researchers can identify suitable candidates for trials more efficiently and monitor their responses to therapies in real time. This not only accelerates the research process but also enhances the safety and efficacy of new treatments by ensuring that they are tested on the right populations.
Furthermore, AI-driven tools are enhancing the patient experience by providing more accessible healthcare solutions. For example, telehealth platforms powered by AI can offer personalized recommendations based on a patient’s unique medical history and current health status. This integration of AI into telemedicine is particularly valuable in neurology, where ongoing monitoring and adjustments to treatment plans are essential for managing chronic conditions.
Despite these advancements, the implementation of AI in neurology is not without challenges. Issues such as data privacy, the need for high-quality datasets, and the potential for algorithmic bias must be addressed to ensure that AI technologies are used ethically and effectively. Continuous collaboration between neurologists, data scientists, and ethicists is essential to navigate these challenges and maximize the benefits of AI in improving patient outcomes.
In summary, the advent of AI in neurology is transforming the landscape of diagnosis and treatment. By harnessing the power of machine learning, healthcare professionals can deliver more precise, personalized care to patients with neurological disorders. As research continues to evolve, the potential for AI to enhance neurological health care remains vast, promising a future where technology and medicine work hand in hand to improve the lives of those affected by neurological diseases.
Telemedicine in Neurological Care
In recent years, telemedicine has emerged as a transformative force in the field of neurology, particularly in the wake of the COVID-19 pandemic. With the increasing need for accessible healthcare solutions, virtual consultations have become a vital tool for both patients and healthcare providers. This section delves into the various ways telemedicine is enhancing access to neurological care and facilitating the ongoing management of neurological conditions.
One of the most significant advantages of telemedicine is its ability to reach patients in remote areas or those with mobility challenges. Many individuals with neurological disorders, such as multiple sclerosis or Parkinson’s disease, often face difficulties in traveling to healthcare facilities. Telemedicine eliminates this barrier, allowing patients to consult with specialists from the comfort of their homes. This increased accessibility not only improves patient satisfaction but also encourages more individuals to seek timely medical advice.
Moreover, telemedicine enables continuous monitoring and management of neurological conditions. Through the use of wearable devices and mobile applications, healthcare providers can track patients’ symptoms and medication adherence in real-time. This data-driven approach allows for personalized treatment plans that can be adjusted based on the patient’s current condition. For instance, a neurologist can remotely assess a patient’s motor function or cognitive performance through video consultations, making necessary adjustments to their treatment regimen without the need for in-person visits.
In addition to improving access and ongoing management, telemedicine fosters a collaborative approach to care. Neurologists can easily consult with other specialists, such as psychologists or rehabilitation experts, to provide comprehensive care for patients with complex neurological conditions. This interdisciplinary collaboration is crucial, as many neurological disorders require a multifaceted treatment strategy that addresses both physical and mental health aspects.
Furthermore, telemedicine can significantly reduce healthcare costs for both patients and providers. By minimizing the need for travel and in-person appointments, patients can save on transportation expenses and time off work. For healthcare facilities, telemedicine can streamline operations, allowing for more efficient use of resources and potentially reducing wait times for appointments.
Despite its numerous benefits, telemedicine in neurology does face challenges. Issues such as technology access, patient privacy, and the need for reliable internet connections can hinder its effectiveness. Additionally, some neurological assessments may require in-person evaluations for accurate diagnoses. However, as technology continues to advance, solutions to these challenges are being developed, making telemedicine an increasingly viable option for neurological care.
In conclusion, the integration of telemedicine into neurological care represents a significant advancement in how patients receive treatment. By enhancing access, facilitating ongoing management, and promoting collaborative care, telemedicine is reshaping the landscape of neurology. As we move forward, it is essential to continue exploring innovative technologies that can further improve patient outcomes and ensure that all individuals have access to the care they need.
Frequently Asked Questions
- What are neurological diseases?
Neurological diseases are disorders that affect the nervous system, including the brain, spinal cord, and nerves. They can impact various functions such as movement, cognition, and sensation, leading to a wide range of symptoms.
- What are some common types of neurological disorders?
Common neurological disorders include Alzheimer’s disease, Parkinson’s disease, multiple sclerosis, and epilepsy. Each of these conditions has unique symptoms and treatment options, making awareness crucial for early intervention.
- How do lifestyle choices affect neurological health?
Lifestyle choices like diet, exercise, and mental health play a significant role in neurological health. A balanced diet and regular physical activity can enhance brain function and potentially reduce the risk of developing neurological disorders.
- What innovative treatments are available for neurological diseases?
Innovative treatments such as gene therapy, stem cell therapy, and neurostimulation techniques are emerging in the field of neurology. These approaches aim to address the root causes of neurological diseases and improve patient outcomes.
- How is technology changing neurological care?
Technology, including artificial intelligence and telemedicine, is revolutionizing neurological care. AI helps analyze patient data for personalized treatment, while telemedicine improves access to care, making it easier for patients to manage their conditions.